New research builds on previous work to identify a link between microplastic pollution and antibiotic resistance.
Tiny microplastics may be contributing to a much bigger problem: antibiotic resistance.
That’s according to new research published in the Journal of Hazardous Materials. The study, led by Dr. Pedro Alvarez of Rice University in the United States, builds on previous work that has suggested links between the oft-invisible plastic particles and the global health problem of growing resistance to antibiotics.
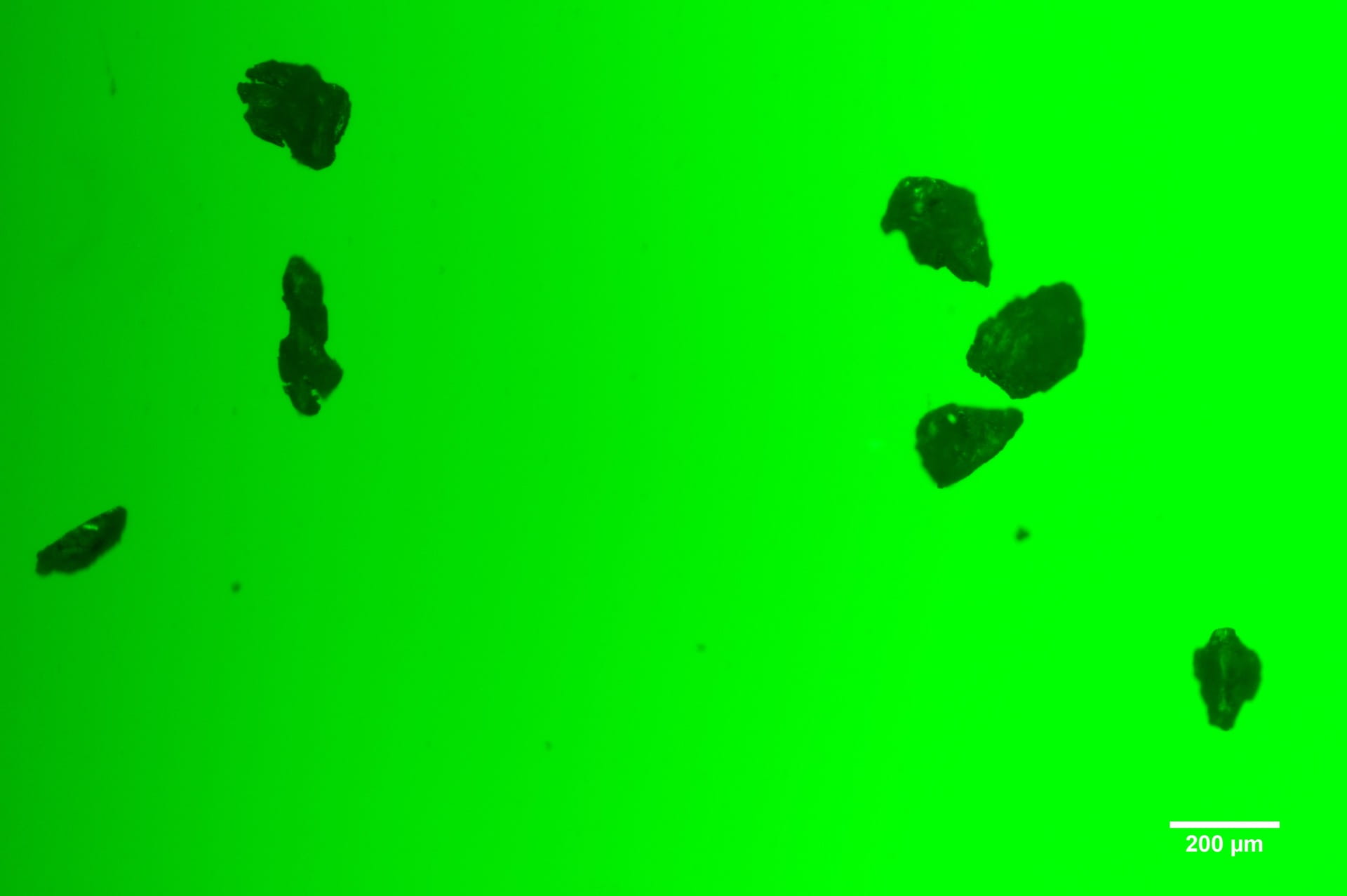
Alvarez and team members from China as well as the University of Houston wanted to see what happens when microplastics begin to age in direct sunlight. They found that particles measuring between 100 nanometers and five micrometers, exposed to ultraviolet rays, trap microbes on the plastic surface.
As the plastic degrades, it also leaches chemicals that break down cell membranes in the microbes. The process makes them even more open to antibiotic-resistant gene (ARGs) development.
The scientists used particles of polystyrene, the plastic resin used to make packaging peanuts or single-use coffee cups. In one example, material aged for 20 days was 6.6 times more likely to absorb common Escherichia coli (E. coli) bacteria. This increased its ability to promote the spread of antibiotic resistant genes.
“Microplastic surfaces may serve as aggregation sites for susceptible bacteria, accelerating gene transfer by bringing the bacteria into contact with each other and with released chemicals,” the authors explain. “That synergy could enrich environmental conditions favorable to antibiotic resistance even in the absence of antibiotics.”
The small changes in the genetic material of bacteria and fungi can make them resistant to existing antibiotic drugs. For example, the World Health Organization (WHO) estimates that in 2018, a half-million people had new cases of tuberculosis infection that no longer responded to the drug rifampicin.
“Without effective tools for the prevention and adequate treatment of drug-resistant infections and improved access to existing and new quality-assured antimicrobials, the number of people for whom treatment is failing or who die of infections will increase,” says WHO. The global health entity has declared antimicrobial resistance (AMR) a Top 10 global public health threat.
But until recently, the researchers said, few people have paid any attention to the microplastics link. Alvarez, who found his team’s results surprising, said this potential impact of microplastics has gone overlooked even though many people are aware of the plastic pollution problem overall.
A Chinese-led study, published in February, found a similar microplastics problem with antibiotics that might enter the food chain via the aquaculture industry, first affecting marine life and then perhaps humans.
A third study, from the New Jersey Institute of Technology, warns that wastewater treatment plants—where 2 million microplastic particles are dumped every day in a city the size of 400,000 people—may become hotspots of antibiotic-resistant pathogens.
“Previously, we thought the presence of antibiotics would be necessary to enhance antibiotic-resistance genes in these microplastic-associated bacteria,” said its lead author, Dung Ngoc Pham. “But it seems microplastics can naturally allow for uptake of these resistance genes on their own. The presence of antibiotics does have a significant multiplier effect, however.”
The studies all call for more attention to the role of microplastics in facilitating antibiotic resistance.
This story first appeared on Sustainability Times
South Africa Today
© 2021 Sustainability Times.
This article is licensed under a Creative Commons Attribution-ShareAlike 4.0 SA International License.